Source: Getty Images
I was 36.
I got breast cancer.
I found it myself.
I knew there was an increased risk, as my mom had had it. I had been doing self-examinations for several years, and knew to look for signs. This time, I just knew it felt different. I listened to my body and called my OB/GYN.
A few days later, a well-meaning, well-trained breast cancer specialist walked into a waiting room, told my husband I had breast cancer, and that I would be getting a mastectomy and simultaneous reconstruction. “Call the office. Buy my book. Goodnight.”
My husband had to tell me that I had cancer, and then take me home to our three-year-old son, and seven-month-old baby daughter.
The words “you have breast cancer” forever changed me.
There is the initial disbelief and then the profound, down-to-the-bones knowledge that life is utterly beyond our control and, at times, sucks.
I had a toddler and an infant and breast cancer. There are no words.
Much like my experience with postpartum depression and my work as a birth doula, breast cancer gave me the opportunity to learn a great deal about the need to advocate for myself and transform the difficulty to help others.
Not to take care of women in an all-knowing, dare I say patriarchal, way that suggests I know your experience. I can’t tell a woman what it feels like to birth; I can’t tell you what it feels like to have breast cancer when you are lactating.
So, rather than grow more fear of the unknown with this entry, I want to plant seeds of power in anyone who needs some words of encouragement.
Look
Look at your body – your amazingly capable, ever-changing body.
Look with awe at its ability to create, heal, and give us direct information about what it needs.
Look to your changing body with courage to see its signals.
Get in there and do your self-examinations.
The answers about what to do will come. Then do it.
Go have a trained professional look at your body and help you with it.
Our bodies never lie.
Listen
Listen to what your care providers say. Carefully.
Write it down. Have your partner write it down.
Listen carefully to what they don’t say. Lots of answers come from spaces in between medical science and your life.
Listen to your intuition. Write that down, too.
When my surgeon told me I was going to have reconstruction through a method that would require me to not pick up my baby for 6-10 weeks, and sounded positively medieval, my instinct said, “You are going to what?”
Even though he posed it as a positive “I will give you a nice tummy-tuck and new boobs,” my instinct told me to learn more. Quickly.
Learn
Learn about it.
Learn what the language means. What are those terms? What is that procedure they are telling you they are going to do?
Don’t just Google it – that’s not good enough. Go to reputable sources of evidence-based information. Universities with research programs are a good place to start, search PubMed, or Wiley Science with your words. You can even ask someone to do it with you.
With my cancer, I assumed what my surgeon was telling me about reconstruction was part of the treatment. Then, like learning the terms and philosophies of childbirth, I learned the language of reconstruction and breast cancer –and discovered that my surgeons’ reconstruction procedure was elective.
He assumed I would want to do it. Multiple surgeries, chance of necrosis, not lifting anything heavy for 6-10 weeks just to have boobs – not my choice.
I was determined to hold my baby and my son as soon as possible.
Plus, the thought of having skin grafted from my labia to create “nipples” was all I needed to re-think the whole thing, okay?
I remember sitting on the porch when I called my OB/GYN, who had just delivered my daughter, and had walked me fearlessly through postpartum depression with my son, and asked, “Do I have to do that?”
No.
She assured me my surgeon would be supportive. She was right.
Reconstruction, with an infant and a toddler, didn’t work for me. So off they went, and the convenient all in one tummy-tuck never happened! (What am I, anyway, Jiffy Lube?)
Lean In
Once you learn what you are facing, my deepest heartfelt advice is to lean into it, and lean on strong things that can really hold you up.
Just as I ask my clients about who can really, really hang in there in the operating room if there is a need for a C-section, I suggest finding those who can face breast cancer with you, and lean on them.
With every wave of fear, or doubt, lean on those supports.
Don’t white knuckle it; don’t rob yourself of the help and support you deserve, and quite frankly, will need.
Lean on your partner, lean on others who have been through it. Lean on your spirituality or religion if you have one. And when in doubt, lean on yourself.
Leaning in doesn’t mean giving up. It means surrendering to the experience with the knowledge that you will come out the other side with grace, and grit.
Laugh Out Loud
Let yourself laugh at the absurdity what your body comes up with, and what the universe brings you in the form of care-providers’ quirks.
I remember my surgeon showing me and my husband how flexible he was – and he was serious! He kicked off his man-clogs right there in the exam room and practically went into full down-dog.
And another time, he made a muscle like Pop-eye and insisted I feel his bicep. So bizarre, it was hysterical.
And speaking of down-dog, I couldn’t help but laugh out loud when I tried wearing prosthetics to yogaand one fell out on my mat. Plop!
Let yourself laugh. It’s okay.
Realizing you will never wear a tube top in public again is not necessarily a bad thing when you are pushing 40. I’m just saying…
Let It Go
Let your life change.
Don’t expect it to stay the same.
Your friends will change. Some will stop calling, some will send a card and then not include you in girl’s night anymore.
It is hard, and sad. Let it go.
Those who don’t know how to love you through a life changing event feel horrible. They wish they could make eye contact with you at Starbucks, and they know in their hearts they hurt you because they fell out of your life when you needed them.
Their loss. Let them go. You will be there for them when they need you.
Family members – those who should know better and still fail miserably –let them go, too.
Neither my mother nor father attended my births, or my mastectomies.
For a long time, I tried to pretend I was okay with it. I wasn’t. I am not. They should have been there for all of it – physically there to hold my hand, my babies, and my fear.
If this happens for you, I am so sorry.
Know that they don’t mean harm. They just have lost the ability to know they are important agents for healing in the world. Sad, really.
And if you are a family member, go be with her. It counts.
Let Your Body Change
It isn’t pretty, but opening to its changes will bring you tremendous relief and insight: You are not your body.
I had one mastectomy at a university hospital and the other at a local hospital. If I were my body, more specifically my breasts, where am I now? Would I exist in two different hospitals? How could my children still love me if I didn’t exist?
Letting go of the wrong view that I was somehow the same as the breast tissue was probably the most healing part of recovery.
—
“When we meet our children, when we hear we have cancer, reality dissolves; we stare mortality itself in the face, and fully dilate at the awesome fragility of life”.
These words are true for birthing our babies, and birthing our cancer.
Lean into yourself; learn the lingo; look without fear at what your body gives you, and let yourself change.
Our lives are fragile and funny, our bodies are stunningly obvious, our spirits surpass any medical procedure.
And as we survive it all, tell your women to do the same.
Want to discuss this further? Login to our online forum and start a post! If you’re not already registered as a forum user, please register first here.
Walker Karraa, PhDc is a doctoral candidate at Sofia University, where she is finishing her dissertation study of the transformational dimensions of postpartum depression. Walker was the founding President of PATTCh, an organization founded by Penny Simkin dedicated to the prevention and treatment of traumatic childbirth. Walker is the perinatal mental health contributor for Lamaze International’s Science and Sensibility, Giving Birth With Confidence, and the American College of Nurse-Midwives (ACNM) Midwives Connection. She is co-authoring a book with Kathleen Kendall-Tackett, Ph.D., IBCLC, FAPA on PTSD following childbirth. Walker is a 10 year breast cancer survivor, and lives in Sherman Oaks, CA with her two children and husband.
Search our 3000+ articles!
Read our articles about:
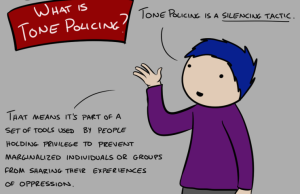
Our online racial justice training
Used by hundreds of universities, non-profits, and businesses.
Click to learn more