A close-up on a stressed-looking person with their legs drawn up to their chest and their chin resting on their knee.
(Content notice: eating disorders, including descriptions of restriction and binging/purging)
When I was a kid, my mom used to joke that none of us could possibly have an eating disorder, because we weren’t in the right tax bracket.
She was (half) kidding, but the sentiment reflected decades of stereotypes about who struggled with disordered eating patterns and painful relationships with food and weight.
At 19 years old, when my mind was threaded through with numbers – my weight, my bank balance, my next payday, my tips, and my caloric intake – I would become quite sure that in fact, you did not need to have a red cent to your name to feel like the only thing that mattered was retaining the tight grasp you had on what you did or didn’t eat.
But as a poor person with an eating disorder, I was also absorbed in guilt.
Any food I wasted by purging just looked like dollar bills in the toilet bowl, and skipping meals was optimal because it saved both money and calories. When the leftover pastries at work were supposed to be bagged up and thrown out, I’d sneak them home – only to spend the evening pacing, staring, and desperately trying not to eat them.
Though we’ve been conditioned to see eating disorders as an affliction of the upper class, in reality, plenty of individuals who are living in poverty are also grappling with the added stress, shame, guilt, and health side effects of eating disorders.
And when the stereotypes about who “can” experience an eating disorder are perpetuated, it can have real-life consequences.
Here are some ways to untangle the relationship between poverty and disordered eating.
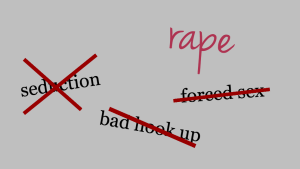
1. Eating Disorders Aren’t Just for Rich White Girls
There are a number of myths about eating disorders.
The general public tends to believe that they’re about weight loss, that they’re only experienced by women, that most who live with them are white (and thin, never fat), and especially that they are strictly the purview of people who live above a certain income level.
None of these things are true – and the root of the myth of eating disorders as a wealthy white cis woman’s ailment is more nefarious than many people realize.
Eating disorders of all forms are certainly not new. Anorexia nervosa was first given a name in 1873, but behaviors that looked like it – as well as those that looked like binge eating disorder, bulimia nervosa, orthorexia, and other disordered eating patterns – have been documented for centuries.
However, it wasn’t until the 1970s that eating disorders began to gain attention among the general public, thanks to a handful of case studies and books released over the span of just a few years – specifically Eating Disorders: Obesity, Anorexia Nervosa, And The Person Within and The Golden Cage by psychoanalyst Dr. Hilde Bruch.
Although she has been called a pioneer in the field of eating disorder studies, she introduced many of the tropes we still associate with eating disorders.
Her work at Baylor University treating patients with eating disorders focused exclusively on women, as many believed (and still do) that men aren’t impacted by eating disorders. (It must be noted that “transgender” was still a new term in the ‘70s, and “cisgender” wouldn’t be coined until the ‘90s, so transgender, non-binary, and intersex identities weren’t even considered. More on that in a moment.)
Additionally, access to psychiatric care was largely limited to wealthier families, which remains the case.
The resulting demographic of Dr. Bruch’s research, then, as well as most that came before it, was unsurprisingly almost exclusively white and middle-upper class. But rather than seeing this population as a portion of those affected by eating disorders, Dr. Bruch’s research pool led her to conclude that eating disorders were exclusive to that group.
Not only that, but she also furthered the assumption that those factors – whiteness, wealth, and cis womanhood – created eating disorders.
“During the 1950s, it was acceptable to be a compliant, nice, sweet girl. If she was bright enough, and from the upper class, she was supposed to go to college and meet a nice Harvard man and settle down,” Dr. Bruch wrote in The Golden Cage:
Now this same girl goes to college to write a PhD thesis and get a job in Washington. Girls with conforming personalities feel obliged to do something that demands a great degree of independence in order to be respected and recognized. When they get stuck, the only independence they feel they have is to control their bodies.
Dr. Bruch also asserted that “the illness goes together with the women’s movement, because this is what the girls want: to show that they are something special.”
Four decades later, the study of eating disorders in groups other than wealthy white cis women (because of course, people of all genders – including trans and nonbinary folks – have eating disorders and yes, they are deeply under-studied) remains “in its infancy,” according to Northwestern University’s Marian Fitzgibbon and Melinda Stolley, who note that
as the field of eating disorders has evolved, researchers and therapists have begun seeing a number of changes, [including] an increase in eating disorders among men… And despite the common wisdom that [women of color] have a kind of cultural immunity to developing eating disorders, studies indicate that [they] may be just as likely as white females to develop such debilitating problems.
Indeed, there are numerous studies that indicate that eating disorders of all stripes are prevalent across demographics (though some are more likely to present in some ethnic and religious groups than others).
So, what accounts for the persistent stereotypes about who “does” and “doesn’t” live with eating disorders?
2. Poverty and Eating Disorders Feed Each Other – No Pun Intended
Just as poverty is an intersectional issue, so too are eating disorders.
That is to say, the outside forces associated with income inequality, access to medical care, the historic trauma of racism, rape culture and sexual violence, and many other deeply damaging systems which push people to the margins also create, trigger, and worsen eating disorders.
For the purposes of this article, I’ll be focusing mostly on the intersection of poverty and eating disorders, though there’s plenty to be said and considered about how eating disorders and race, orientation, gender, religion, immigration status, and incarceration all impact a person’s experience with disordered eating.
There’s a documented connection between the stress of poverty and poor mental health. In general, people living in poverty are more likely to experience depression and other mental illness, or to see exacerbated symptoms of an existing illness. Eating disorders are no exception.
Eating disorders, though, collide with poverty in unique and troubling ways.
We’ve moralized the hell out of food and food choices, determining that almost without exception, the most affordable and accessible foods (think: things you’d find at a bodega) are also the ones that tend to be the considered the “worst.”
Limited access to abundant, affordable food choices can leave to added shame and guilt. Fitness deserts – areas without the infrastructure for affordable exercise – make it difficult for low-income people to work out regularly, particularly in areas where luxury fitness outfits are popping up like dandelions.
The realities of poverty and eating disorders are often at odds with each other.
During the most poor period of my adult life, I remember wandering my local corner store with an exact amount of cash I could spend, conducting what seemed like an impossible calculation: how to find foods low in calories and high in protein while still maximizing the value of my money.
Because I’m a vegetarian, this was nearly an impossible task. I ended up shoplifting some almonds I couldn’t afford and living off those for a day or two.
Many behaviors that we might associate with both frugality and “healthy” eating practices, like buying in bulk, limiting portion sizes, and cutting out extras and treats, can also be eating disorder symptoms.
My trips to the Grocery Outlet to buy cases of inexpensive, low-calorie protein bars weren’t just in response to my financial constraints: It was because I was obsessed with saving money and counting calories, and good old Grocery Outlet just made it easier to accomplish both.
And of course, saving money by skipping meals is perfectly acceptable if you’re poor, right?
On the other end of the spectrum, eating disorders that include binging or obsessive eating patterns (issues like orthorexia, which is most colloquially described as being consumed by a need to eat “pure” or “clean” foods) may be costly to maintain, which can cause further strain on a person living in poverty.
And because poverty and the medicalization of fat (and “obesity”) are also fairly intimately linked, eating disorders among people living in poverty often fly under the radar.
Though the common understanding of eating disorders (not to mention the DSM description for anorexia nervosa) is that they’re primarily about weight loss, the truth is that many eating disorder behaviors will not result in weight loss.
In fact, plenty of eating disorders actually result in weight gain, which means our cultural beliefs about who is suffering may make it difficult to see the reality of the lived experience.
Additionally, eating disorders manifest differently in different ethnic and social groups, which are disproportionately impacted by poverty.
In immigrant communities, for example, some cultural norms may be extremely triggering. There’s also some research that shows that some eating disorders are more prominent in LGBTQIA+ communities. And individuals from different ethnic groups have shown to be more prone to some kinds of disordered eating than others.
The relationship between eating disorders and poverty is also circular: Cis women who have eating disorders have been shown to earn less money and may even end up out of a job if they become too overwhelmed or physically unable to work.
Medical bills – whether it’s for hospital stays, dental work, or even broken bones as caused by osteoporosis – can deepen debt and wring a person dry.
That is, assuming they feel like they can seek care at all.
3. Treatment Is Expensive and Difficult to Access
At the lowest low of my eating disorder, I remember lying in my bed with my laptop propped up beside me, exhausted and in pain, surfing message boards that purported to be about recovery, but were definitely a trigger-farm.
One thread was about a documentary that was on YouTube that featured women at an inpatient treatment center.
I watched it, transfixed. Their lives seemed so simple. They didn’t have to go to work. They didn’t have to go to college. They were just there. Being sick. Getting help.
I was awash in envy. At the time, I was holding down two jobs while attending school full-time; I was very, very broke and disconnected from the majority of my friends and family. I was also completely wracked with a combination of undiagnosed ADHD, bipolar, and an eating disorder.
In the documentary, it became clear that expense actually was an issue. One woman was discharged early because her insurance ran out.
I looked up the average cost of inpatient treatment and was floored: a month of residential treatment can cost up to $30,000 – more than the annual poverty threshold for a family of five.
Even if a person can get treatment, either through the ACA or Medicaid – both of which still offer much less comprehensive coverage than the best insurance in the world, which is just having a ton of money – the care they receive varies based on the disorder, the person, the culture, and the provider.
Not only are health care providers generally worse at spotting eating disorder symptoms in people of color, patients themselves may also often have a hard time identifying them.
Which is a long way of saying: Poor folks typically don’t get treated for their eating disorders, which means the stereotype that they don’t have them at all is permitted to persist.
***
Living in poverty already has a tendency to create a tenuous relationship with food, health, and resources – at least, it did for me.
And the many ways that we stigmatize and moralize the food choices and options that low-income folks face only serve to exacerbate the problem.
Until we collectively acknowledge that mental health issues like eating disorders impact people of all stripes, those who are suffering will continue to do so alone.
[do_widget id=’text-101′]
Hanna Brooks Olsen is a Contributing Writer for Everyday Feminism, a small human, and a Millennial. Her interests are politics, podcasts, Pac-12 football, feminism, and Oxford commas. She is curious to a fault. Follow her on Twitter @mshannabrooks.
Search our 3000+ articles!
Read our articles about:
Our online racial justice training
Used by hundreds of universities, non-profits, and businesses.
Click to learn more